Anterior Minimally Invasive Surgery (AMIS)
Hip Replacement Technique
NO muscles cut!
Much lower risk of dislocation
Small incision
Dr Freeman teaches at special training courses for this technique and is the most experienced surgeon in Queensland able to offer this technique. He has been performing AMIS since 2009 and has completed more than 500 hip replacements using the AMIS technique. Surgery is available at John Flynn Hospital on the Gold Coast.
History
The anterior approach to the hip joint was first described by Hueter in 1881. It was initially used for draining infected joints.
French surgeons used the anterior approach with the first total hip replacements in 1949 and continue up to the present day.
Prof. Frederick Laude in Paris adapted the approach in 2004 ago and modified the traction table and tissue retractors to create a truly "minimally invasive approach" to the hip for joint replacement. His approach was termed AMIS (Anterior Minimally Invasive Surgery).
Over 200,000 AMIS total hip replacements have been performed world-wide since 2004.
New?
The specific technique, including how the tissues are handled, how the retractors are placed and how they are used, to result in less tissue damage whilst performing a safe operation, is the important difference to other methods.
The device which holds the leg and allows it to be moved around and provide traction, developed by Prof. Laude, is a great aid during surgery with this technique. It reduces the risk of fracturing the leg, replaces one medical assistant, does not block the blood flow to the leg thus reducing the risk of deep venous thrombosis (blood clots), and enables the operation to be more comfortably performed on all sizes of patients.
Features
Surgical Approach
 Only a small skin incision is needed to provide a good view for the surgeon, unlike previous "mini incision" approaches which had a poor view and significantly increased the risks of complications.
Only a small skin incision is needed to provide a good view for the surgeon, unlike previous "mini incision" approaches which had a poor view and significantly increased the risks of complications.
The AMIS incision is only 5-7cm in length, whereas antero-lateral or posterior approach incisions are usually 15-30cm in length!
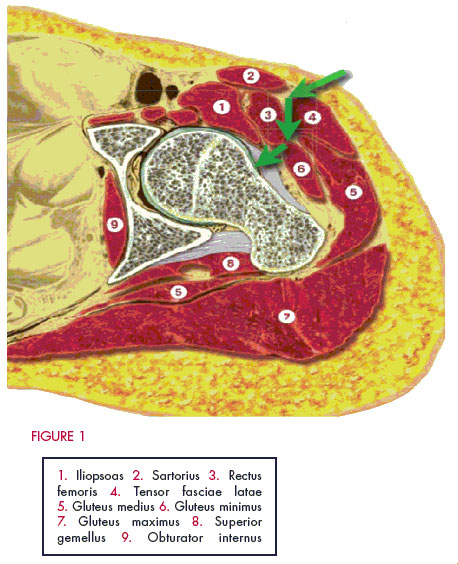
With AMIS there is no detachment, splitting or denervation of muscle. No muscles are cut as they are simply retracted to create a gap. The tensor fascia lata muscle is retracted laterally whilst the rectus femoris muscle is retracted medially. There is no gluteal (buttock) muscle injury with this approach.
The gluteal muscles provide the main hip power and stability, and as they are entirely intact with the AMIS approach a faster recovery is expected. The posterior or antero-lateral approaches cut through the buttock muscles and tendons even with the so-called mini-incisions or mini-invasive operations.
The AMIS approach enters between the nerve supply to the muscles so the muscle fibres retain their full ability to function after the operation. Other approaches permanently damage either muscle fibres and/or the nerves which supply them, so there may be a permanent loss of nerve function and/or partial muscle wasting.
The Traditional Two Approaches
Antero-lateral
- The hip abductor (gluteus medius and minimis) muscles/tendons are detached and split, frequently resulting in a permanent limp as they are unable to stabilise the hip after the operation. Bone lumps often grow in the damaged gluteus muscle.
- The Superior gluteal nerve which supplies the muscles is at significant risk of traction injury resulting in permanent weakness.
- Cut through the tendons of gluteus maximus and tensor fascia lata muscles.
Posterior
- The gluteus minimis muscle is cut off the capsule often resulting in lumps of bone growing in the muscle after the operation. Has the highest risk of dislocation but usually no limp after surgery.
- Cut through the tendons of gluteus maximus, tensor fascia lata, piriformis, gemelli and obturator muscles.
- Risk of sciatic nerve injury with "mini" incision.
Protection of Tissues
AMIS is "minimally invasive" as it is designed to result in the absolute minimal damage to tissues and structures surrounding the hip joint.
Retraction of the muscles is with the tough hip joint capsule, which is preserved. The sharp edges of the metal retractors may cause muscle tears with other techniques.
The gluteus minimus muscle is not cut or damaged, thus minimizing the risk of heterotopic ossification (lumps of bone forming in the muscle) after the surgery which could permanently restrict the joint movement.
A combination of the above features is expected to result in :
- Decreased post-operative pain
- Shorter hospital stay
- Faster return to daily activities
- Higher level of function
and has resulted in those parameters in my patients compared to those who previously had the posterior approach.
All patients who had previously had a lateral or posterior approach hip replacement have preferred the AMIS approach after their surgery on the other hip.
It is now rare for abdominal or minor joint surgery to be performed by "open procedures" due to the advantages of minimally invasive "laparoscopic" and "arthroscopic" surgery. The principle and philosophy of using the AMIS technique is analogous to modern laparoscopic and arthroscopic surgery by aiming to achieve :
- Small wound
- Good view
- Minimal "collateral" tissue damage, especially to nerves and muscles
- Safety
- Faster recovery
- Lower post-operative complications
MRI (magnetic resonance imaging) scans of the muscles after AMIS show a normal muscle appearance. MRI scan after other approaches demonstrates permanent muscle damage with scarring and wasting of the muscle fibres, which presumably results in a permanent reduction of function and strength (which is particularly relevant as patients age and become weaker, even if they were relatively young and strong at the time of surgery).
Safety
Dislocation
- AMIS dislocation is reported as 2 in 1,000 (0.2%).
- Anterolateral and posterior approach dislocation rates are reported between 10 and 50 per 1,000 (1 to 5%).
Therefore the risk with AMIS is between 5 and 20 times lower chance of dislocation than with the other approaches – which is a major difference.
As recurrent dislocation of the hip joint is the 2nd most common reason for re-operation, the AMIS approach significantly lowers the risk of further surgery for this problem.
Revision surgery takes longer, has higher risks of infection and blood clots, costs more, plus causes further tissue damage, and is therefore highly is desirable to avoid.
As the AMIS approach significantly reduces the risk of dislocation it is worth seriously considering the AMIS approach simply to reduce the risk of revision surgery.
Nerves
The AMIS approach is between the nerve supply to the muscles and therefore the muscles will be able to resume their full function after surgery.
The major nerve trunks (femoral and sciatic) are at least a full muscle thickness away from the surgery with AMIS and therefore have a minimal risk of injury.
The sciatic nerve is particularly at risk with the posterior approach and may even be injured by greater than normal bleeding after the surgery has been completed.
The superior gluteal nerve is at high risk with the anterolateral approach, which may result in long-term hip instability due to loss of gluteal muscle power.
Prostheses (implants)
Have been used since 2005, although prostheses of a similar design have been used for more than 30 years.
The latest and strongest bearing materials are normally used. "Delta" ceramic is 10 times stronger than the previous alumina ceramic.
Ceramic has the lowest wear rate and also causes the lowest immune reaction to the wear particles. It has the greatest potential to last longer than other materials and result in the fewest number of surgeries for revision of the prostheses.
Highly cross-linked polyethylene has been specially treated and is also available. This has a much lower wear rate than the old plastic bearings.
Other Features
No post-operative restrictions as required with other approaches.
Permited with AMIS
- allowed to bend down (arms between knees)
- sit with the hips flexed greater than 90 degrees (although it is prudent to ensure knees are 40cm apart)
- no need for a toilet seat raise.
- able to lie on either side immediately post-op:
- wound is anterior and therefore no direct pressure on wound or operation area;
- less problems with pressure area care as patients do not have to lie only on their back;
- improved sleep, especially for patients with sleep apnoea who have problems always lying on their back;
Better leg position during surgery and increased early post-operative mobility lowers the risk of DVT (blood clots).
Lower risk of infection as there is only a small cut which is away from the perineum.
Well proven, with over 200,000 operations using this technique. It is not experimental or a gimmick, but is established now, and is the future too.
No need to travel interstate to have this surgery, plus local aftercare and follow-up on the Gold Coast.
We have extensive experience with managing patients from long distances, including regional areas of Queensland and New South Wales, plus other states and territories.




